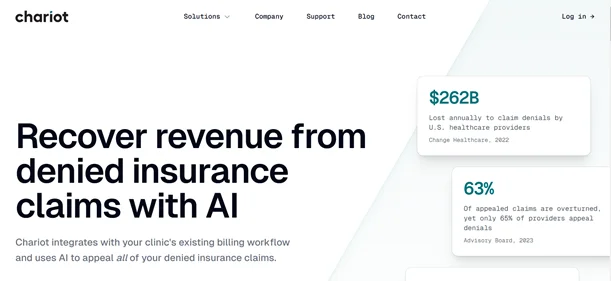
In the complex landscape of healthcare billing, denied insurance claims can significantly impact a clinic’s financial health. Chariot AI addresses this challenge by automating the appeal process.
It connects with your current EHR or billing systems without disrupting your workflow, ensuring a smooth integration.Once connected, Chariot AI examines denied claims to uncover common denial reasons and errors.
It then amends these discrepancies, compiles the required documentation, and resubmits the claims in accordance with payer guidelines. This automation not only streamlines operations but also offers insights to help prevent similar denials moving forward.